HMO, PPO, EPO or POS? Choosing a managed care option
There are a lot of factors to consider when you’re shopping for individual health insurance coverage – from premiums to deductibles to on-exchange and off-exchange and ACA-compliant (or not). If you’re shopping in the individual health insurance market, you’ll definitely be making a choice of metal tier.
And – regardless of where you shop – you’re going to end up making a decision about a type of managed care that works best for your situation. As you’re selecting a health plan – whether it’s ACA-compliant or not – you’ll notice that the plans are labeled as either an HMO, PPO, EPO, or POS.
These acronyms stand for Health Maintenance Organization, Preferred Provider Organization, Exclusive Provider Organization, and Point of Service. They are categories of managed care, which is how virtually all modern health insurance is organized.
(The alternative is an indemnity plan, which doesn’t have a provider network. Indemnity plans are almost unheard of in today’s major medical health insurance market.)
Why do health plans have managed care designations?
Managed care is a medical delivery system that attempts to manage the quality and cost of medical services that individuals receive. Each type of managed care limits, to varying degrees,
the number of providers from which a patient can choose,
whether the patient has to use a primary care physician, and
whether out-of-network care is covered under the plan.
Some managed care plans attempt to improve health quality, by emphasizing the prevention of disease.
Indemnity plans – popular before the advent of modern managed care plans – have been largely replaced by managed care plans over the last several decades, and the vast majority of privately insured Americans are in some form of managed care plan.
Even in the Medicaid and Medicare systems, managed care is playing an increasingly large role: More than two-thirds of the Americans enrolled in Medicaid were covered under private Medicaid managed care plans as of 2019. And more than 45% of Medicare beneficiaries were enrolled in private Medicare Advantage plans as of early 2022 – a percentage that has been steadily growing over the past decade.
What’s the difference between an HMO, PPO, EPO, and POS plan?
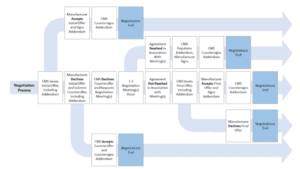
To a large degree, the differences involve access to providers. All HMO, PPO, EPO, and POS plans have networks of medical providers (doctors, hospitals, etc.) that have a contract with the health plan in which the carrier agrees to accept a negotiated price for the services they offer. Some plans will only pay for non-emergency care if you receive care from an in-network provider, while other plans may cover some of the bill if you see an out-of-network provider.
You’ll often see simple comparison charts that show the “rules” for the different types of managed care. In a nutshell, they’ll generally say that HMOs and POS plans require a referral from a primary care doctor in order to see a specialist, while PPOs and EPOs do not, and that PPOs and POS plans cover out-of-network care, while HMOs and EPOs do not. They will also often tend to say that HMOs have lower premiums, lower deductibles, and smaller provider networks, while PPOs have higher premiums, higher deductibles, and broader networks.
In reality, the lines tend to be more blurry, and these types of plan management have evolved over time. For example, this POS plan from Blue Cross Blue Shield of North Carolina does not require a referral to see a specialist. Neither does this HMO from Friday Health plans. And while it’s often true that employer-sponsored HMOs tend to have lower deductibles and premiums and potentially smaller networks, that does not hold true in the individual/family (self-purchased) market.
It is generally true, however, that EPO and HMO plans will not cover out-of-network care unless it’s an emergency, while PPO and POS plans will provide some out-of-network coverage. But the out-of-pocket costs for out-of-network care will typically be substantially higher than the out-of-pocket costs for in-network care. For example, that POS plan from Blue Cross Blue Shield of NC has an in-network deductible of $8,700 for a single individual, but an out-of-network deductible of $43,500. And this PPO, offered by Ambetter in Oklahoma, has an in-network deductible of $8,600, but an out-of-network deductible of $20,000.
So although PPO and POS plans do generally “cover” out-of-network care, you might find that you only get a benefit from that if your out-of-network costs are particularly high. And it’s also common to see that plans with out-of-network coverage do not put any cap on total out-of-pocket costs for out-of-network care.
(The ACA requires health plans to cap out-of-pocket costs for essential health benefits obtained from an in-network provider – the cap is $8,700 this year – but there are no limits on how high out-of-network costs can be, even if the plan provides out-of-network coverage.)
Plans with lower deductibles are certainly available, although their premium costs are generally higher. But they will still tend to have much higher out-of-network deductibles. For example, this Medica PPO has an in-network deductible of just $750. But the out-of-network deductible is $9,900, and again, there is no cap on how high out-of-pocket costs can be for care received outside the plan’s provider network.
Should you consider managed care designation?
When you’re shopping for a health insurance plan – either through the health insurance marketplace or off-exchange – there are many factors to keep in mind. (This is also true if you’re selecting from among options offered by your employer, although there are likely to be far fewer choices in that case.) We’ve covered some of them here, and also have a detailed summary of things to keep in mind when deciding which metal level is right for you.
So should the HMO, PPO, EPO, or POS designation matter when you’re selecting a plan? Maybe, but it’ll depend on the specifics of the plans that are available to you and the coverage details that are important to you.
In general, you’ll want to have a general understanding of the different types of managed care, and understand whether your choice will include any coverage for out-of-network care (that’s generally only available on PPOs and POS plans). And you’ll want to make sure you understand whether your health plan will require referrals from a primary care provider. But as described below, there are several points to keep in mind as you’re comparing plans.
Availability of managed care options varies by location
First, it’s important to note that the availability of the various managed care options differs quite a bit from one area to another. In general, when we look at individual/family plans available through the marketplace, POS plans are very rare, and PPO plans are much less common than HMOs and EPOs.
But in some areas (Wyoming and Alaska are examples), all of the available plans are PPOs. In other areas, the only available plans are HMOs and EPOs, meaning that there are no options that provide coverage for out-of-network care.
To give you an idea of how this varies from one area to another in the marketplace, there are, as of 2022:
129 HMOs and 5 PPOs available in Chicago
Only HMOs available in Atlanta
127 EPOs and 66 HMOs available in Orlando
84 EPOs and 80 HMOs available in Dallas
3 HMOs and 24 PPOs available in Billings, Montana
65 HMOs, 3 PPOs, and 10 POS plans available in Raleigh, North Carolina
15 EPOs and 6 PPOs available in Birmingham, Alabama
24 HMOs and 40 PPOs available in Tulsa, Oklahoma
10 HMOs, 33 PPOs, and 33 EPOs available in Minneapolis
25 HMOs, 5 EPOs, and 10 PPOs available in Los Angeles
So where you live will determine which types of managed care plans are available to you. Once you know what’s available, you can certainly take the managed care designs into consideration.
Four managed care considerations
But there are several factors to keep in mind:
1. Make sure you understand your plan’s coverage of out-of-network care
Although a PPO or POS plan will “cover” out-of-network care, it’s important to understand how that works. Be aware of the deductible (which is likely to be quite high) and the out-of-pocket exposure (which could be unlimited).
Also be aware of the fact that an out-of-network provider can and will balance bill you unless it’s an emergency or an out-of-network provider working at an in-network facility. (Here’s how the No Surprises Act protects consumers from surprise balance bills in those situations).
This means that although your health plan may pay for some of the service (assuming you’ve met the out-of-network cost-sharing requirements), the provider can bill you for the portion of their charges that were above the amount the health plan paid.
2. Narrowness of networks varies
All four types of managed care plans can have broad, narrow, or mid-size provider networks. Don’t assume anything. Instead, you’ll want to actively compare the provider networks of each plan you’re considering, to see whether your specific providers are in-network.
If you don’t currently have any providers, it’s a good idea to see whether each plan you’re considering has in-network hospitals and medical offices that would be convenient if you ended up needing medical care.
3. Managed care is different in the individual market
Individual/family plans aren’t the same as employer-sponsored plans, and that includes the provider networks and managed care rules. You may have had an employer-sponsored plan offered or administered by a particular insurer, but don’t assume that individual/family plans from that insurer will have the same provider network or managed care rules (for example, whether or not a referral is required).
4. Referral requirements vary
Although you may have heard that HMOs and POS plans require a referral from a primary care physician in order to see a specialist, that’s not necessarily true. Again, you’ll need to check the specifics of the plans you’re considering. (And there are pros and cons to referral requirements. On one hand, they mean an additional office visit, which adds to your costs. But on the other hand, your PCP can help to ensure that you’re seeing the correct specialist, and can coordinate the care you receive from multiple specialists.)
Referrals are sometimes confused with prior authorizations (pre-authorizations), but those are two different concepts. A referral comes from a primary care physician, whereas prior authorization has to be obtained from the health plan itself. Health plans can set their own rules in terms of which services require prior authorization. All four types of managed care plans — HMOs, PPOs, EPOs, and POS plans — can and do require prior authorization for various services. But there’s a lot of variation from one plan to another in terms of what services need prior authorization.
So it’s important to understand your plan’s rules, and to ensure that your doctor has your health plan information so that they can submit prior authorization requests on your behalf. And if in doubt, it’s best to contact your health plan before a particular service is scheduled, to make sure you know whether prior authorization is necessary, and if so, whether it has been granted.
An HSA is not a type of managed care
If you’ve read this far, you may be wondering why a health savings account (HSA) isn’t listed here. It’s common to see comparison charts that include PPO, EPO, HMO, POS, and HSA (Health Savings Account). That leads many consumers to assume that the HSA acronym is a form of managed care – but it’s not.
HSA-qualified high-deductible health plans (HDHPs) allow enrollees to contribute pre-tax money to an HSA (you cannot contribute to an HSA unless you have active coverage under an HDHP). And HDHPs must conform to specific IRS rules. The IRS sets minimum deductibles and maximum out-of-pocket limits (which are lower than the maximum out-of-pocket limits that HHS sets for other plans), and limits the services that the plan can pay for before the deductible is met.
However, HDHPs can be PPOs, EPOs, HMOs, or POS plans. So this is an “and” scenario, rather than an “or” scenario. An HDHP will also be either a PPO, HMO, EPO, or POS plan.
The HDHP designation means that the plan conforms to the IRS rules for HSA-qualified plans. And the HMO, PPO, EPO, or POS designation describes the plan’s approach to managed care.
Don’t hesitate to ask questions about your managed care options
As always, you can turn to a broker or navigator if you need assistance with the process of comparing health plans and picking the one that will best meet your needs. Depending on when you’re applying for coverage, our guide to open enrollment and our guide to special enrollment periods will answer many of your questions.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org. Her state health exchange updates are regularly cited by media who cover health reform and by other health insurance experts.