Backend Process for LOAs
Note: This is a provider question. Please let me know if I should redirect this to a different subreddit.
I'm hoping to get some insight on the process behind the scenes of getting a Letter of Agreement from someone who's worked on the backend (UM/Contracting/etc.) at an IPA or Health Insurance plan.
Here's the situation. We are a provider (California) who has received an authorization from an IPA that we are not associated or contracted with. We are contracted with the Health Plan for this particular patient. Per the DOFR, the IPA is responsible for both authorizations and claims for this particular service. This service does not have a fixed reimbursement rate. I've always been under the assumption that when requesting a Letter of Agreement from an IPA, since they are receiving capitated payments from the Health Plan, the IPA just does a Letter of Agreement (contract) with the provider requesting the LOA. Today, I spoke with a rep that informed me that there's another layer of contracting that happens between the IPA and the Health Plan in order to provide that LOA, even though the DOFR has already assigned the IPA as responsible for this particular benefit.
Basically:
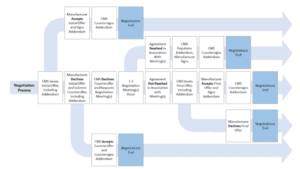
An outside provider requests an LOA with the responsible party (The IPA) The IPA then requests some sort of permission (contract?) with the Health Plan to be able to provide the LOA to the outside provider Presumptively, the Health Plan gives some kind of permission for the IPA to go ahead and provide an LOA The IPA then writes up the LOA and sends it back to the outside provider
I was not aware this extra layer existed. Can anyone explain to me how this process works? Is my understanding of the process correct? What is the purpose of the Health Plan signing off on IPA LOAs when they're already financially responsible for this service? Any additional information on how this all works would be greatly appreciated. 🙂
submitted by /u/miss-moxi
[comments]