[WI] Transitioning from workplace insurance coverage to COBRA
My situation is a big mess but heart of my question is: Is being covered under COBRA insurance the same as being on my workplace's insurance policy, with the entire premium cost being paid by me (and my deductible and out of pocket max accumulations being preserved)?
My employer is Wisconsin based and I currently live and work in Wisconsin.
I have been undergoing cancer treatment since July 2023, which was initially covered under a plan period of 7/1/23-6/30/24. I was not covered under federal FMLA (hours worked) and applied for ADA leave. They claimed it as "personal leave" and were going to "close out my employment" after two months. I returned to work the first week of October 2023. During the period I was out, I wrote my employer a check for my portion of the benefits that could not be deducted as I had no paycheck coming in. My out of pocket max of ~$7k was was met by the end of July under this plan.
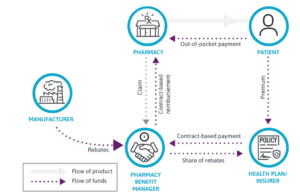
In January 2024, we were forced into a new open enrollment for a plan effective 3/1/24-2/28/25. My employer had now elected to self-insure and was utilizing a benefit manager. In January imaging showed that it my cancer may have not completely respond to first line treatment and that I may need further treatment after a new biopsy. While the new plans being offered included a no deductible option, my cancer center was not in network, so I had to choose the plan option that had similar deductible and OOP max as my previous plan. This effectively caused me to lose 4 months of "free" healthcare because the previous plan was being termed. Sucks, but nothing I could do about it.
Further treatment has been needed and I'm headed towards a stem cell transplant. While the claims have not been fully adjudicated yet (yay, Change Healthcare hack…), I have likely met my OOP max again. My healthcare provider is saying I need to be out of work for a minimum of 6 months for this portion of the treatment plan. Instead of approving any further leave, my employer wants to change my employment status from part-time to pool. I asked how this benefits me – return to my previous status/hours after treatment? Continued support in the form of my employer a portion of my benefit premiums? Obviously, the answer to both questions were both "No." This feels akin to constructive dismissal or just a way for my employer to save face by not firing a long time employee for cancer. They have issued me COBRA paperwork terming my workplace plan 4/30/24.
My other questions related to this situation:
My HR department is saying because I am not out on protected FMLA leave, I would be responsible for the full premiums. This was not the case during my leave in 2023. I imagine this may be different between organizations, but is this true/common? Losing this coverage would be a qualifying event. My husband has plan (effective 1/1/24-12/31/24) that has a similar deductible and OOP max. The monthly cost to add me to his plan would be similar to what my COBRA payment would be. Because of have (likely) already met my OOP max, it would make the most sense to choose the COBRA option instead of partner's plan – correct? Related to the question at the top of my post – because my employer's transition to self insuring, if I elect to choose the COBRA coverage, are they still responsible for paying for my treatment or do my claims get shifted to another fund?
I'm angry and upset, and realize a lot of this is a venting post, so if you've read this far, thank you! I appreciate any insight that you might be able to provide. Additionally, if you think there is another location that would be better able to provide answers to my questions, feel free to direct me there.
submitted by /u/sigsbee
[comments]